what is a biopsychosocial
December 13, 2020
There have been many shifts in thinking with regards to our understanding of pain.
.webp?width=776&name=601245afb6dedc3ba8d1da15_SUNDAY+READINGS+(2).webp)
The Evolution of Our Understanding of Pain
There have been many shifts in thinking with regards to our understanding of pain: Aristotle thought pain was “passion for the soul”. Rene Decartes thought that pain was the result of the tubes conveying liquids to our brain. More recently, Pat Wall and Ronald Melzack came up with the Gate Control theory. Our most recent view on pain is drawn from multiple fields and domains and is seen as an emergent process - many things come together, all at once and pain emerges out of the “chaos”.
For the past century or so, medicine and healthcare have been administered primarily within a Biomedical framework when addressing pain. This framework is mostly focused on the biology, anatomy, pathology, and disease process occurring in an individual. And it is originally derived from the Germ Theory of disease, which postulates that all disease is a product of a biologic defect often initiated by a biologic pathogen. Unfortunately this model is overly simplistic and reductionist, seeking to explain all disease in biologic terms.
This model served its purpose however and was largely successful...for a while. At the beginning of the 20th century, the leading causes of death were tuberculosis, pneumonia, influenza, and diarrhea. For acute injuries and disease, a Biomedical approach can be very fruitful. By the end of the 20th century however, people died of chronic disease - heart disease, cancer, and stroke. Now Americans continue to die primarily from chronic disease. Almost one in two U.S. adults has a chronic disease, and treating chronic illness accounts for 75% of our health care costs.
The Biopsychosocial Model of Pain
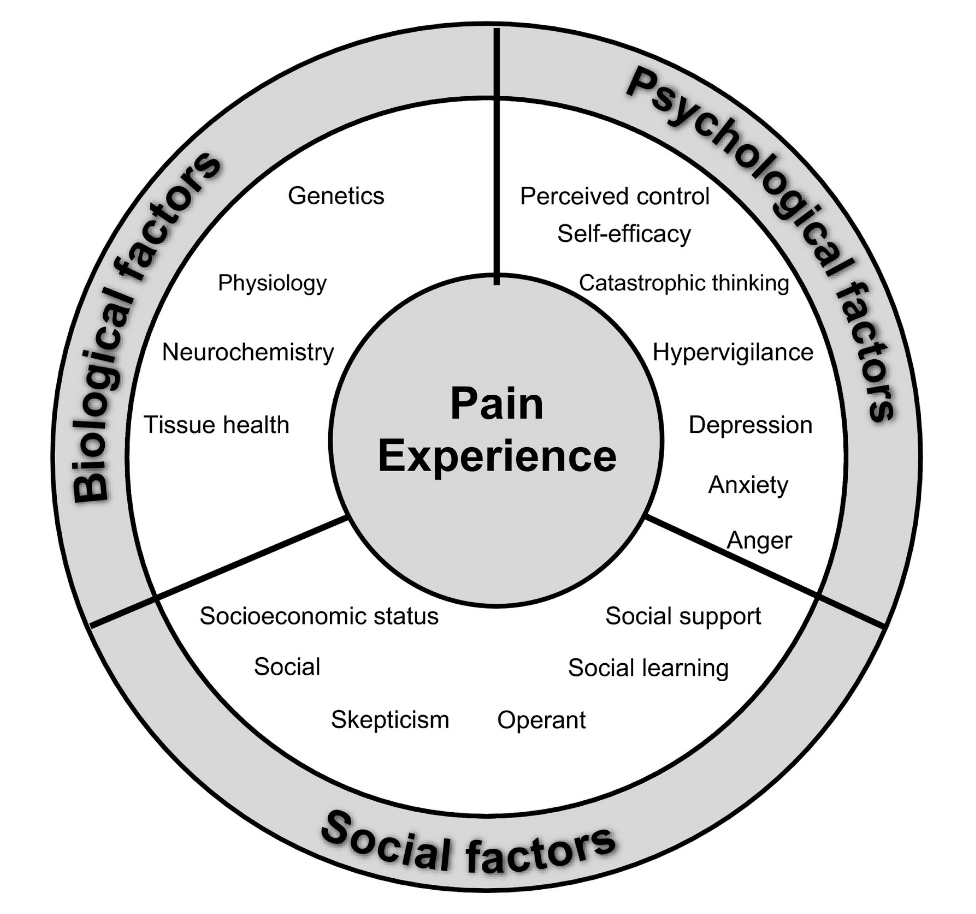
The response to these changes has been a shift away from the Biomedical model and towards the Biopsychosocial, which emphasizes the processes that occur within an individual and their environment. It emphasizes three overlapping domains of biology, psychology, and society and recognizes that processes in each of those three domains interact with each other to determine health and wellbeing, as well as poor health, disease and illness. Although this paradigm shift has been taking place for a little while now, the emergence of the Biopsychosocial model of care is now at the frontier of medicine, where it belongs.
This means that in all of healthcare and specifically within Physical Therapy, we need to be taking a more holistic approach when it comes to treatment and management of patients. To reiterate, pain is an emergent phenomenon and not a linear one. A linear process would imply that if A, then B - it is an organized and structured process that occurs in a strict sequence. We view pain as being more emergent, meaning that many things come together, all at once and then pain rises out of the chaos. In other words, that chronic low back pain probably had more to do with a confluence of factors across multiple domains rather than that singular event where you bent over to tie your shoes. That may have been the proverbial straw that broke the camel’s back however, no pun intended.
How Does MOTIVNY Use the Biopsychosocial Model of Pain?
If you check out our previous upload to the journal by Luke, you can see how we may take various psychosocial factors into consideration such as an individual’s perception of their pain and their motivation behind avoiding, enduring, or embracing their symptoms and the feedback of their body. So don’t be surprised when you are being asked seemingly random and unrelated questions to your specific pain because they are not (i.e. stress levels, work, relationships, etc). Being more mindful of the person in front of us and not just their physical body leads to more successful outcomes. This means quicker turnarounds, more educated and empowered individuals, and lessons that lead to more long term success and longevity as well...one of the pillars of the MOTIVNY philosophy.